ASHEVILLE, N.C.—Bianca Davidson was 17 and still in foster care when she got pregnant. The baby, a boy, arrived a month-and-a-half early, and no one warned Davidson that being premature put him at risk for life-threatening illnesses and developmental delays. She hemorrhaged after delivering her second son, but the doctor simply told the nurses to “clean her up.” A family member insisted to staff that something was wrong and a second doctor ordered blood transfusions. “It was super-scary,” Davidson, 29, recalled. “Nobody talked me through … ‘Ok, you lost a lot of blood so you can’t be with your baby at the moment.’” Her third pregnancy, three years later, required an emergency caesarean section when her son’s heartbeat dropped suddenly. Davidson was afraid the next time she gave birth, either she or her baby would not survive.
She had good reason to be afraid.
According to the Centers for Disease Control and Prevention, black women across the country are 320 percent more likely to die from pregnancy-related complications than white women. In Buncombe County, where Asheville is located, black babies were nearly four times as likely as white babies to die before their first birthday. These woeful statistics cut across economic and educational lines, as pregnant black women with a college degree die at five times the rate of their white counterparts. Experts say the causes are complex and bound up with the stress of living in a society that discriminates against people of color—from a lack of diversity in the medical profession to implicit bias in the way providers treat patients. In 2017, the American College of Obstetricians and Gynecologists said maternal health disparities “cannot be reversed without addressing racial bias,” adding that “structural and institutional racism contribute to and exacerbate these biases.”

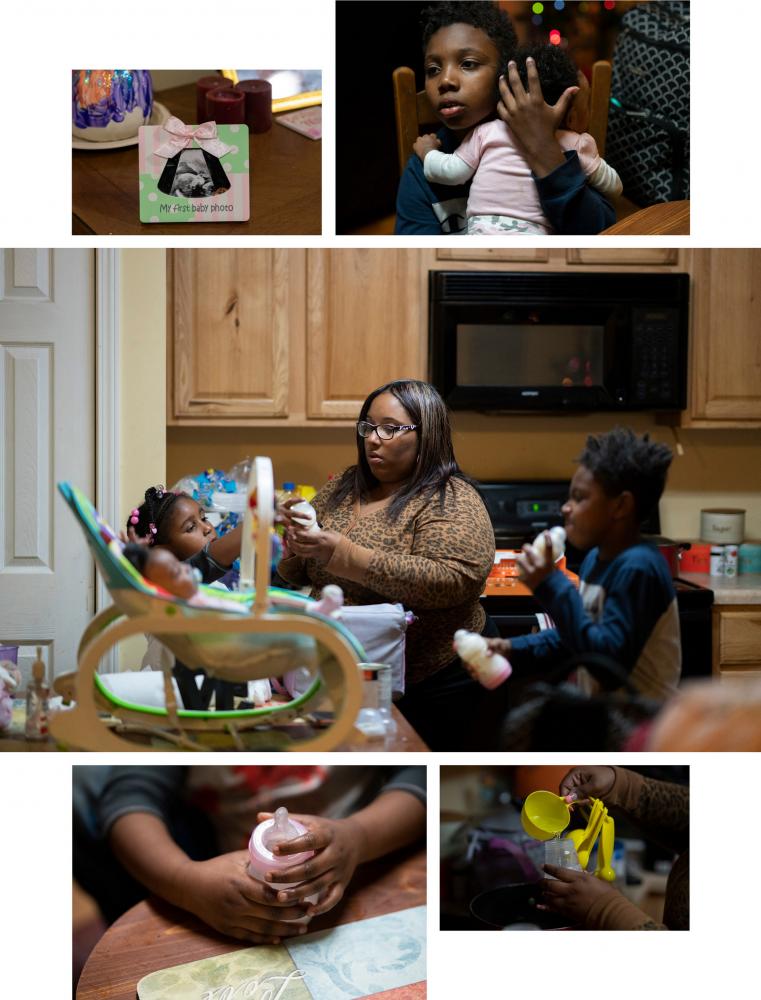
Bianca Davidson, 29, has a healthy 3-month-old daughter named Kahlani Durrah, that she delivered with the help of doula Wakina Norris, 51. | Photograph by Melissa Lyttle
In early 2019, when Bianca Davidson was pregnant with her fourth child, she was uncertain about how to protect herself. She went to a prenatal appointment at the Mountain Area Health Education Center, a non-profit founded 45 years ago to train doctors in the western part of the state. Its obstetrics and gynecology clinic serves most of the pregnant women in the region who are uninsured or on Medicaid. About 2,900 women received prenatal care at the Asheville center last year, and most of them delivered their babies at nearby Mission Hospital.
Davidson had been to the clinic for her first pregnancy, but this time her doctor offered her a service that wasn’t available 12 years ago: a doula. She wasn’t sure what a doula was. Davidson works as a cashier at Burger King and lives in a public housing complex near downtown. So Wakina Norris made an appointment to meet her at MAHEC, introduced herself, and explained that doulas provide non-medical physical and emotional support to women before, during and after childbirth. They don’t deliver babies like midwives but they are there to help women get through it. “I was intrigued by it,” Davidson said.
Norris, 51, is one of three full-time members of Sistas Caring 4 Sistas, a doula program run by and for black women. The doulas are employees of the Mountain Area Health Education Center who provide free support to high-risk, low-income mothers like Davidson. Unlike most doulas—who are predominantly white and upper middle-class like their clients—these women understand intimately what it means to give birth in a country where the color of a woman’s skin can determine the quality of her medical care.

A group of 22 women go through a three-day Homegrown Babies Doula Training program together at the Buncombe County Partnership for Children in Asheville, North Carolina. | Photo by Melissa Lyttle
After their first meeting, Norris visited Davidson at home and accompanied her to some of her prenatal appointments. Davidson confessed that she was scared, and unsure how to handle another labor. When the doctor told her she might need to have another caesarean section, she balked. She knew other women who had delivered vaginally after a C-section, and she hoped to do the same. “If that’s what you want to do, we’re gonna do it,” Norris told her. She wrote down Davidson’s birthing plan and brought it with her to the hospital this summer when Davidson went into labor.
Studies show that doulas help reduce the rate of caesarean surgeries, which is higher among black women than other racial groups, and other costly interventions. Doulas also increase the rate of breastfeeding, which improves the health of new moms and babies and is less common among black or low-income women. They can even alleviate some of the socioeconomic factors that contribute to poor maternal health, such as limited access to education or social support networks. “They play this role in leveling the playing field a little bit,” said Rachel Hardeman, an assistant professor at the University of Minnesota School of Public Health who has studied doulas extensively. Yet only 6 percent of American women give birth with the help of a doula. Their services are not usually covered by insurance and can cost $700 to $1,500 per birth.
Awareness of the health crisis facing black women has grown nationally but the solutions to it so far have been primarily local. Private groups such as Ancient Song Doula Services have been providing doulas to women of color in Brooklyn for a decade, and similar groups have launched in cities such as Austin and Atlanta, where the National Black Doula Association is based. In the past six years, New York, Oregon and Minnesota have expanded their Medicaid programs to cover the cost of doulas for qualified patients. Baltimore and Milwaukee now offer free or reduced-cost doulas to low-income women and people of color.

At the Homegrown Babies Doula Training program, women learn about the power of touch, and consent, by asking if it's ok if they touch their client and where it hurts, so they can help minimize their pain. | Photographs by Melissa Lyttle
Programs like these can make a difference. The 90 clients served by Sistas Caring 4 Sistas from May 2018 to May 2019 were 12.4 percent more likely to get prenatal care in their first trimester than other black women in Buncombe County in 2018. Only 6.8 percent of black children born within the doula program were low birthweight compared to 12.7 percent of black children born in the county overall. None of the infants in the program died, while two of the 181 black children born in the county died in 2017.
Experts say community-based doulas cannot, by themselves, overcome all the complex factors that contribute to higher mortality rates for black mothers and their babies; legislation needs to be part of the solution. Obstetricians advocate expanding Medicaid coverage for new mothers beyond two months postpartum. Last year, Senator Kamala Harris (D-California) introduced the Maternal CARE Act, which would provide funding to address implicit bias among medical students, and grants to states that provide comprehensive, culturally competent care to high-risk pregnant women. The bill was reintroduced this year, but never made it out of committee.
“Policy has to be addressed, systemic racism has to be addressed,” said doula Cindy McMillan, the education and marketing director for Sistas Caring 4 Sistas. “But until all these things happen, we’re just there to help them advocate for themselves.”
This July, with Norris by her side, Davidson had her first trauma-free birth. When the painful contractions mounted in the delivery room, she anxiously pleaded with the doctor to “cut me open.” Norris gently but firmly reminded her that was not in her birthing plan. Davidson had made it clear that she wanted to push—and she did.
Her daughter, Kahlani Durrah, arrived after 17 hours of labor without surgical intervention. Norris was with her the whole time. “It was a nice experience having somebody there who was willing to advocate for you,” Davidson said. “Because there’s times when the doctors will override what you say—to do what they need to do, or [to] make it easier on them.”

Cindy McMillan at Pisgah View Apartments. | Photographs by Melissa Lyttle
‘Nobody should go through that alone’
Sistas Caring 4 Sistas was born out of the pain of the women who founded it.
The idea began in 2016 at the Pisgah View Apartments, a public housing development in Asheville where Norris and McMillan’s sister, Nikita Smart, lived. The Mountain Area Health Education Center was hoping to apply for a grant from the Blue Cross and Blue Shield of North Carolina Foundation that funded collaborations between a medical clinic and the community it served. So the center sent two employees to Pisgah View for more than a year to sit at picnic tables in the middle of the complex and listen to the women who live there. They formed close bonds with Norris and Smart, who was already working at the Pisgah View resource center, helping arrange GED and typing classes for residents. Smart invited McMillan to join them. Together, the women discussed how stress was affecting their health. They planned a spa day for mothers in the complex, complete with acupuncture, massage and doulas from Homegrown Babies in Asheville.
The owner of Homegrown Babies decided that day that if they would have her, she wanted to teach the women from Pisgah View her skills. “I saw that there was no diversity within this field,” said Chama Woydak, who has been a doula in Asheville for 20 years. As McMillan and the other women learned how modern doulas could help combat the county’s black infant mortality rate, they embraced the concept. “We were really upset,” McMillan said. “This is a personal attack on us, on black women.”
The techniques they learned from Woydak, from birthing positions to massage, often felt familiar, given how much they had supported laboring relatives in the past. Norris has four children and six grandchildren and used to work as a certified nursing assistant. “I was a doula before I was a doula,” she said. Black women have a long history of supporting each other through childbirth. “Granny midwives,” as they were known, delivered babies of all races throughout the rural South until the mid-20th century, when birth became more medicalized fewer women had babies at home.
After the doulas were trained and certified by DONA International, the largest certification organization for the profession, they considered starting their own businesses and accepting private clients through Homegrown Babies. But that was a daunting prospect in a county where just 6 percent of the population is black. When Homegrown Babies held a “meet the doulas” event for prospective clients, Smart and her colleagues were the only people of color in the room. To Smart, it felt like “walking into a roomful of white people and putting yourself on glass and saying ‘Hi, ‘I’m for sale.’”
So the women decided to work together as Sistas Caring 4 Sistas. They still accept some private clients, but primarily work at MAHEC. The center made combating black infant mortality the centerpiece of a grant proposal, partnering with Buncombe County and non-profits in the area on an effort called Mothering Asheville. A portion of the $150,000 in annual funding pays the doulas $15-an-hour plus benefits. It’s not a lot for a job that can require 18 hours on your feet with a woman in labor—but none of the doulas chose this path for the money.

Top: Nikita Smart, left, pictured with Shae Wright. Below: Pisgah View Apartments, Asheville, North Carolina's largest public housing complex. | Photographs by Melissa Lyttle
Seventeen years ago, McMillan gave birth to twin boys in St. Petersburg, Florida. After a C-section, she awoke from the anesthesia feeling like hot blades were slicing through her abdomen. She tried to yell, then started hemorrhaging. “The doctor told me that if I didn’t stop bleeding, then I wasn’t gonna make it,” McMillan said. “He told me to stop bleeding.” McMillan resented the implication that she was somehow responsible for the situation. As she lay fighting for her life, she learned that one of her twins needed a blood transfusion due to a heart defect. The doctor saved McMillan, but her baby died before she left the hospital.
McMillan wanted to file a complaint against the doctor and spoke to lawyers about her situation. She requested medical records and says the hospital refused to provide them. Finally, in 2010, she gave up. The lack of documentation makes it difficult to confirm the details of what occurred, but her experience echoes that of many black women.
In a recent survey of 2,700 women of all races across the country, 22.5 percent of black women reported being mistreated by a healthcare provider during pregnancy or childbirth. Women of color were twice as likely as white women to report “that a health care provider ignored them, refused their request for help, or failed to respond to requests for help in a reasonable amount of time,” the study states. Separate studies show that black people are undertreated for pain in America. Postpartum hemorrhaging is one of the leading causes of pregnancy-related death in the U.S., and black women who experience it are at higher risk of serious injury or death than their white counterparts.
Black women are also more likely to have conditions that put them at risk for pregnancy complications, such as hypertension and fibroids—non-cancerous growths in the uterus. The past president of the American College of Obstetricians and Gynecologists has said doctors are missing the opportunity to treat these issues before a woman becomes pregnant, and before they threaten her life.
Public health professionals are beginning to connect the health of black women with the negative effects of living in an unequal society. Arline Geronimus, a professor at the University of Michigan School of Public Health, calls the phenomenon “weathering.” Geronimus found that black women age faster and develop chronic diseases such as hypertension earlier, due to the stress of living in a society that discriminates against them.
The doulas in Sistas Caring 4 Sistas have experienced the consequences of that inequality personally. McMillan’s goal is to make sure her clients never feel as powerless as she did. “If you don’t feel heard, you don’t want to waste your words,” she said. “You look at a lot of the women who passed away after giving birth, a lot of them went to their providers and said, ‘Something wasn’t right. Something wasn’t right.’ And they sent them home.”
After Wakina Norris’s second pregnancy, her doctor told her she didn’t need to have any more children. He convinced her to have her tubes tied when she was 24 years old. “That was a form of racism. I just didn’t think about it,” Norris told me. “I wanted a big family, but it was stopped because I trusted that individual.”
Smart labored by herself when she had her daughter in 2003—a common experience among women the doulas now serve. The Florida hospital where she gave birth assigned her a “sitter,” a woman who Smart says barked orders at her, telling her not to push and to stop screaming. “Nobody should ever have to go through that alone,” Smart said. “If I can make sure nobody else has my birth story, then I’ve accomplished something.”

Family photographs of Karima Hemphill. | Photographs by Melissa Lyttle
Filling a gap of missing family
One evening in late August, I followed McMillan as she drove through the gentrifying heart of West Asheville, past the tea room and co-op bookstore, until the landscape transitioned to strip malls. She turned north, past a handful of churches scattered between homes on winding mountain roads. We climbed a steep, pockmarked driveway to a cluster of two-story houses with vinyl siding and wooden porches. This was a routine home visit for McMillan to check on Karima Hemphill, a client who had a C-section scheduled in two weeks. The doulas make prenatal and postpartum visits to ensure their clients have enough food, clothing and other supplies, set up birthing plans and provide emotional support.
Inside, family photos decorated the entrance wall to Hemphill’s tidy living room, while the dryer clanked noisily in a closet. Hemphill’s daughter, who is 4, greeted us holding a framed picture of her late grandmother and ordered us to take off our shoes. Her 11-year-old brother was outside playing with kids from the neighborhood.
Hemphill, 28, explained that she was initially skeptical of hiring a doula when a friend suggested it, even though she works as a business office specialist at MAHEC and knew about the Sistas Caring 4 Sistas program. “She didn’t trust me,” McMillan said. “I liked it though, ’cause she got to feel me out. Now she invites me to lunch. I feel like I graduated,” she added, with a hint of pride and teasing in her voice. “I got invited to her baby shower and everything.”
Karima Hemphill and her children at home. | Photographs by Melissa Lyttle
Hemphill discovered she was pregnant just as the baby’s father, who is now incarcerated, was facing a court trial. McMillan boosted her spirits and encouraged her. “She’s so positive,” Hemphill said. Hemphill worried about who would be with her in the delivery room. “I been so stressed out about that,” Hemphill said, explaining that her mother died when she was young and she’s not close with her sister. “My suggestion was to have someone that’s not going to elevate stress,” McMillan said. Hemphill picked McMillan.
Like many of the doulas’ clients, Hemphill has a history of pregnancy complications. When she was about three months pregnant with her daughter, she went to church one morning and felt a pinching in her lung. It hurt to take a deep breath. She hurried to the emergency room, and the doctors told her she had a urinary tract infection. “I’m like, ‘a UTI?’” Hemphill remembers thinking. “I said that it hurts when I breathe.”
So her sister called her father, and he in turn lectured the doctors about the family’s history. “Her mother died of a pulmonary embolism and you need to figure out if she’s got one.” Hemphill heard the doctors protest that they were worried about threatening her pregnancy, but her father stood his ground.
They ran some tests, and Hemphill could hear the doctor exclaim from behind the curtain, “Holy shit! She really had one.” Hemphill now takes injections to prevent blood clots. But when we visited her that evening, she surprised McMillan by mentioning that her supply had run out and she had stopped taking the shots. She just couldn’t stomach injecting herself, she told McMillan.
McMillan told me later this confession worried her. Clients often share such details with their doulas but not their doctors, leaving the doulas to make a judgment call about how to proceed. At her next prenatal appointment, McMillan urged Hemphill to tell her doctor she was uncomfortable taking the shots, and she did. But that night, McMillan kept her concerns to herself. She asked to see the baby’s room instead. Hemphill took us upstairs to show us the bassinet beside her bed, and a closet full of onesies with sayings like “Actual mermaid, just add water.”
As we walked back downstairs, McMillan advised Hemphill to use the first week of her maternity leave to stock groceries, toilet paper, and detergent before the baby arrived.
“You got this,” she said firmly, and Hemphill hugged her goodbye.

LaPorsche McCranie. | Photographs by Melissa Lyttle
‘I am part of a system that’s racist’
Hemphill’s frustration with her medical care is not unique. Indeed, distrust of the medical community among black women has deep historical roots, from the experimental surgery conducted on enslaved women to state-sponsored sterilization that lasted until the 1970s in North Carolina. And it persists today. A 2016 study of 222 white medical students found that half of them believed there were biological differences between black and white people, such as that black people had thicker skin or their nerve endings were less sensitive.
“We hear a lot of our women talk about mistreatment that they’ve experienced in hospital settings during birth,” McMillan said. “You don’t trust the health care system, then you’re not gonna come and be seen and be checked out when it is necessary, because you’re in fear of mistreatment, or judgment, or misdiagnosis.”
Ashley Traynum-Carson, 37, who works in communications for local government in the Asheville area, ran into similar stereotypes last year when she gave birth to her first child. When she went to Mission Hospital because she was having unusual bleeding, the doctor referred to Traynum-Carson’s husband as her “baby daddy.” When she was in labor—vomiting and miserable—it took three hours for Traynum-Carson to receive an epidural injection for pain. (McMillan said she witnessed this as her doula). Traynum-Carson asked for a different nurse but says she was told the hospital was understaffed and couldn’t provide one. It took a team of vein specialists to insert the IV needed for her to receive fluids before the pain medication.
After her daughter was born, Traynum-Carson had trouble breastfeeding. She asked for baby formula because the lactation consultant couldn’t see her until the next day. But when the consultant arrived, she told Traynum-Carson, “You gave her formula, there’s nothing I can do for you,” and offered to sign her up for a Women, Infants, and Children subsidy—akin to food stamps for new mothers—instead. Mission Health’s media relations manager, Nancy Lindell, said the hospital could not comment on individual patients due to federal privacy laws. However, she said the hospital tells all patients about WIC because the annual income threshold to receive it is $39,46 for a family of three. Still, Traynum-Carson knew she and husband made too much money to qualify. “I felt like Mission Hospital just failed me,” Traynum-Carson said.

Doula Wakina Norris does a pre-natal visit at the home of mom-to-be Ashley Williams, 29, who is due in late February 2020. | Photograph by Melissa Lyttle
LaPorsche McCranie, a client of Smart’s, took medication to control her blood pressure when she was pregnant in 2017, but didn’t realize how serious her condition could be. She went for a routine prenatal appointment at 34 weeks and was told she had borderline preeclampsia—a complication marked by high blood pressure that can threaten the life of the mother and baby. The doctors admitted her to Mission Hospital and induced labor. “I was getting really, really scared,” McCranie said. She called Smart at 5 a.m., and the doula stayed with her for the next 13 hours, talking her through each part of the labor process.
When the baby was born, he weighed just 4 pounds. McCranie wanted to hold him on her chest before he was whisked away to the neonatal intensive care unit. Smart made sure the doctors allowed that to happen. Later, when McCranie was in the NICU visiting her son, she overheard a nurse gossiping to a colleague about the reason her baby was premature. “Her chart says blood pressure, but I guarantee if we test this baby, [the test] will be full of drugs,” McCranie recalled the nurse saying.
McCranie was livid, but Smart intervened. “Let’s go,” the doula said. McCranie reported the nurse’s comments to her superior, and the nurse was sent home for the day. McCranie decided not to file a formal complaint, reasoning that “people have bad days.” Lindell could not comment on this specific incident but said in a written statement that umbilical cord toxicology screening “is completed as part of our standard practice on all admissions to the NICU.”
McMillan says assumptions about drug abuse are common among healthcare providers dealing with her black clients. In her view, nurses or doctors think “the only reason you’re behaving or feeling these symptoms...is because for one, you’re black, and two, maybe you have an addiction.”

Doula Cindy McMillan helps lead a group called Mother 2 Mother in the Pisgah View Apartments. | Photographs by Melissa Lyttle
Dr. Beth Buys, director of obstetrics and gynecology at MAHEC, is aware of these and other disparities in the way black women are treated. “It’s pretty clear that there is a difference in who gets a drug screen and who doesn’t,” she said. But as a white doctor she said she didn’t always see those differences.
That changed three years ago at a conference at MAHEC on black infant mortality rates in Buncombe County. She said she had known for decades about the national disparity in infant mortality but seeing the numbers in the county where she had delivered babies for 16 years shook her. “To realize that my best intentions weren’t having an equal outcome was really distressing,” she said. “I’m embarrassed that that’s what it took.”
One of Mothering Asheville’s goals is to change the policies and institutional racism that have contributed to the mistreatment of black mothers at MAHEC’s clinics and Mission Hospital. The doulas are one key component: They educate patients, allowing pregnant women to feel more empowered to direct their own care. A bigger hurdle, Buys said, is helping doctors, nurses, and staff realize they have a pattern of unequal treatment. If racism is embedded in healthcare and throughout society, they are not immune to it effects. “As a provider, even with my best intentions, [I] am actually complicit and part of a system that’s actually racist,” she said.
MAHEC is gathering data about its drug screens and C-section rates so the stats can be used to identify discriminatory patterns and break them. The center already has some rules in place that are meant to override unconscious biases. Given the racial disparity in the life-threatening risk of hemorrhaging, doctors now measure the amount of blood a woman loses during childbirth instead of estimating it. MAHEC has also conducted implicit bias training for doctors in its residency program, teaching them about the history of racism in women’s healthcare and how to combat it.
In a statement, Lindell said Mission Hospital offers “broad-based education for our team members on recognizing unconscious bias and creating a more inclusive environment for all those we serve.” She added that the hospital has worked to improve maternal and infant health by developing “processes for the recognition and treatment of hypertension during pregnancy and adopting a robust process for the management of postpartum hemorrhage.”
Angela Aina, interim director of the Black Mamas Matter Alliance, says her group has seen admirable efforts in residency programs to address health disparities. Yet seasoned doctors, nurses and hospital staff are often left out of racial bias training. That’s why her group advocates for changes in the overall healthcare system. Making community-based doulas and midwives available to more women of color is just one part of that equation, she said. “It really does require a more systems-level approach to really address the structural racism and gender oppression.”

Nikita Smart, a doula, waits for school buses to start arriving, so she can catch up with women and their children who she knows are still living in the complex. | Photograph by Melissa Lyttle
‘I looked at my check and almost cried’
Since their doula training began, the three founding members of Sistas Caring 4 Sistas have moved to Candler, a small town west of Asheville. None of them can afford to live in the city, where rental prices are among the highest in the state. Norris, who lives in a trailer with her husband, drives 25 minutes to Mission Hospital to be with clients who are in labor. Last year, McMillan’s husband died in a motorcycle crash. She became the sole provider for her four children, the youngest of whom is 6 years old. None of the doulas consider $15 an hour to be a living wage.
“I looked at my check this morning and almost cried,” said Smart, who is raising a teenage daughter on her own. She was considering disenrolling from her health insurance program because the benefit took such a large chunk out of her paycheck.
Maggie Adams, the program director for Mothering Asheville, is lobbying for North Carolina’s Medicaid program to cover doula services. That would make Sistas Caring 4 Sistas more sustainable, allowing the doulas to serve more clients and earn at least $1,200 per birth—an improvement over their current hourly rate. McMillan says they are hoping to hire three more part-time doulas in the near future. She’s working to become a certified doula trainer so she can bring more black women into the profession. Meanwhile, she, Smart and Norris are raising funds for a freestanding birth center. They want to expand their operations beyond MAHEC’s doors, giving their clients a comfortable place to go in the early stages of labor, when the hospital would ordinarily send them home.

Bianca Davidson and her daughter. | Photographs by Melissa Lyttle
In mid-October, Bianca Davidson brought her new daughter to MAHEC to visit Norris. Kahlani was three months old and a healthy 13 pounds, wearing a pink bow around her head and a matching pink-and-white onesie. When Norris picked her up, the baby smiled, her round cheeks mirroring the joy on the doula’s face. “She’s so content,” Davidson bragged about her daughter. “She’s definitely my calm child.”
As Davidson described her labor and the support Norris provided, Kahlani sat on Norris’s lap and held her finger. She didn’t fuss or squirm. Gradually, as she listened to her mother’s voice and soaked up her doula’s adoration, the baby fell asleep. She was safe and warm, protected by the women who brought her into the world.
Lisa Rab is a journalist in western North Carolina. Her work has appeared in Harper's and The Washington Post Magazine. Reach her at lisarab.com.


Spread the word